Gut-brain connection plays key role in understanding IBS

Speaking at this year’s Probiota conference, Richard Day, vice president of medical affairs and clinical development at ADM, explained that the company had conducted a three-arm randomized controlled trial administering probiotic and postbiotic versions of Bifidobacterium longum to 200 adults between 18 to 65 years of age who had a diagnosis of diarrhea predominant IBS.
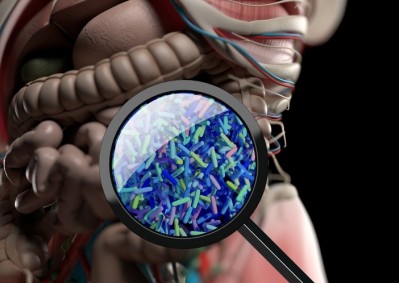
IBS is primarily defined as recurrent abdominal pain related to change in stool consistency or stool frequency. Day estimates it impacts 9% of the world’s population, or approximately 800 million people.
The participants were randomized to receive either the probiotic, the postbiotic or an identical placebo for more than 84 days. The researchers monitored IBS symptom severity score and looked at quality of life measures, abdominal pain scores, stool consistency and even anxiety.
The latter may seem surprising, but Day said a gut-brain component plays an important role in the understanding of IBS.
“When I was at medical school, IBS was taught and conceived as a digestive condition,” Day said. “But now if you talk to gastroenterologists, particularly those who specialize in the treatment of IBS, they will often talk about the fact that it is a disorder of gut-brain interaction. And in fact, if you look at the epidemiology of IBS, we see that there are a lot of comorbidities particularly with anxiety and depression.”
The study by Day and his team, which appeared in April in Gut Microbes, found not only a statistically significant difference between the severity of symptoms between the probiotic, postbiotic and placebo groups (they improved for the experimental groups), but the outcomes were clinically meaningful as well. Quality of life scores also improved for the probiotic and postbiotic cohorts, and they experienced a reduction in stress versus the placebo.
“We have to remember that this particular group was not a clinically anxious population,” Day noted. “So, to see this improvement in anxiety in this population is particularly interesting. And it may also hint at one of the underlying mechanisms of action for both the probiotic and the postbiotic in this population.”
The socioeconomic impact
IBS can have both direct and indirect costs, although health care expenses vary from country to country and can be difficult to track. Day cited a study from the Netherlands in which researchers found that direct costs for IBS sufferers, which included consultations, hospital admissions and medications, totaled €800 (US $860) on a quarterly basis.
However, indirect costs are far greater, he said, adding that these costs are broadly made up of work absenteeism and work presenteeism, or being at work but not being as productive as a person normally would be without symptoms.
“Despite a large amount of research into IBS, currently there's a lack of clear management options available,” Day said.
In recent years, the microbiome has become an important target for research into IBS. The number of PubMed publications related to both microbiome and the condition has steadily increased since the early 2000s. These include interventional studies—often small, randomized, placebo-controlled trials—but also several systematic reviews and meta-analyses of trials.
“What we see is a relatively consistent picture,” Day said. “The microbiome is an important part in the overall picture for irritable bowel syndrome. And what we see across these clinical trials is a generally positive effect for probiotics in IBS.”
However, the microbiome isn't the only important feature when discussing the disorder. IBS is referred to as a multifactorial or complex condition.
“We must remember that this is just one part when we're thinking about the etiology or the pathophysiology of IBS,” Day said.
Source: Gut Microbes
doi: doi.org/10.1080/19490976.2024.2338322
"A randomized double-blind, placebo-controlled trial to evaluate the safety and efficacy of live Bifidobacterium longum CECT 7347 (ES1) and heat-treated Bifidobacterium longum CECT 7347 (HT-ES1) in participants with diarrhea-predominant irritable bowel syndrome"
Authors: S. Srivastava et al.